Vanderbilt Assessment: Beyond ADHD Screening—ODD, Anxiety & Depression
December 25, 2025 | By Nathaniel Pierce
Is your child's behavior more than just typical childhood inattention? The Vanderbilt Assessment is famous for ADHD screening. However, its power goes far beyond attention issues alone. Many parents and educators are surprised to learn this tool also helps identify other conditions. These can include Oppositional Defiant Disorder (ODD), anxiety, and depression. These conditions often appear alongside ADHD or even on their own.
In this guide, we will explore the full scope of this valuable tool. You'll learn how the NICHQ Vanderbilt Assessment Scale provides a complete behavioral picture. Understanding the full range of what is measured can give you clearer insight. If you're ready to better understand your child's behavior, you can start an assessment on our platform.

What Co-occurring Conditions Does the Vanderbilt Assessment Screen For?
While primarily used for ADHD, the Vanderbilt Assessment includes questions that screen for other common behavioral and emotional challenges in children aged 6-12. These are often called co-occurring conditions because they frequently appear with ADHD. Recognizing them is a critical first step toward providing comprehensive support.
Understanding Oppositional Defiant Disorder (ODD) Indicators
Oppositional Defiant Disorder (ODD) is a behavioral disorder characterized by a persistent pattern of angry or irritable mood, argumentative or defiant behavior, and vindictiveness. The Vanderbilt Assessment contains a specific section with questions targeting these behaviors.
Parents and teachers are asked to rate how often a child:
- Argues with adults.
- Actively defies or refuses to comply with requests or rules.
- Deliberately annoys others.
- Blames others for their mistakes or misbehavior.
Elevated scores in this section do not mean a child has ODD. However, they are important indicators that suggest a conversation with a healthcare professional is needed. These behaviors can cause significant problems at home and in school, and early recognition is key.
Identifying Anxiety Symptoms Through Vanderbilt Questions
Anxiety in children can look different than it does in adults. It might appear as fear, worry, or even physical symptoms like stomachaches. The Vanderbilt Assessment includes questions designed to pick up on signs of anxiety.
These questions ask about behaviors such as:
- Being fearful, anxious, or worried.
- Feeling worthless or inferior.
- Seeming self-conscious or easily embarrassed.
- Complaining of physical ailments without a known medical cause.
A child who scores highly in this area may be struggling with an underlying anxiety disorder. Sometimes, these symptoms can be mistaken for inattention, as a worried child may have trouble focusing in class. The assessment helps separate these concerns for a clearer picture.
Recognizing Depression Warning Signs in the Assessment
Childhood depression is a serious but treatable condition. Its signs can sometimes be subtle, appearing as sadness, irritability, or a loss of interest in favorite activities. The Vanderbilt Assessment helps flag these potential warning signs.
The screening questions for depression and mood disorders focus on symptoms like:
- Feeling sad, unhappy, or depressed.
- Losing interest in formerly enjoyable activities.
- Expressing feelings of hopelessness.
Observing these signs can be worrying for any parent or teacher. The assessment provides a structured way to document these concerns, creating a clear starting point for a discussion with a pediatrician or child psychologist. Getting a comprehensive view is easy when you use our tool.
The Hidden Connection: How ADHD and Co-occurring Conditions Overlap
ADHD rarely travels alone. Research shows that a significant percentage of children with ADHD also have at least one other co-occurring condition. Understanding this overlap is vital for creating an effective support plan, as treating only the ADHD may not address the child's full range of challenges.
ADHD and ODD: The Challenging Co-occurrence
The combination of ADHD and ODD is one of the most common co-occurring pairings. It is estimated that up to 40% of children with ADHD also have ODD. The impulsivity from ADHD can fuel the defiant behaviors of ODD, creating a challenging cycle for families.
A child with both conditions might struggle to follow multi-step directions (ADHD) and then argue when redirected (ODD). This can strain the parent-child relationship and create conflict at school. The Vanderbilt Assessment helps identify if both sets of symptoms are present, which is crucial for developing strategies that address both impulsivity and defiance.
When Anxiety Masks ADHD Symptoms (and Vice Versa)
The relationship between ADHD and anxiety is complex. A child who is constantly worried may be too distracted to pay attention in class, looking like they have inattentive-type ADHD. On the other hand, a child with ADHD may develop anxiety because of their academic or social struggles.
Without a structured tool, it can be challenging to determine which condition is primary. Fortunately, the Vanderbilt Assessment separates questions about inattention from anxiety questions. This allows parents and professionals to identify whether one or both areas are a concern, preventing misinterpretation and guiding more targeted support.
Depression and ADHD: Recognizing the Dual Presentation
Living with ADHD can lead to frustration and low self-esteem, which may result in feelings of sadness and hopelessness—hallmarks of depression. Additionally, symptoms can overlap between the conditions, as both can cause concentration difficulties, low motivation, and irritability.
Using a standardized tool like the Vanderbilt Assessment is invaluable in these situations. It allows for a separate look at ADHD symptoms and mood-related symptoms. Identifying this dual presentation is critical, as it often requires a more comprehensive treatment approach that addresses both the ADHD and the child's emotional well-being.
Interpreting Vanderbilt Scores for Co-occurring Conditions
After completing the questionnaire, you will receive a scored report. Understanding what these scores mean is the next step. While a formal interpretation should always be done with a healthcare provider, here is a general guide to help you make sense of the results. To see how it works, you can get started now.
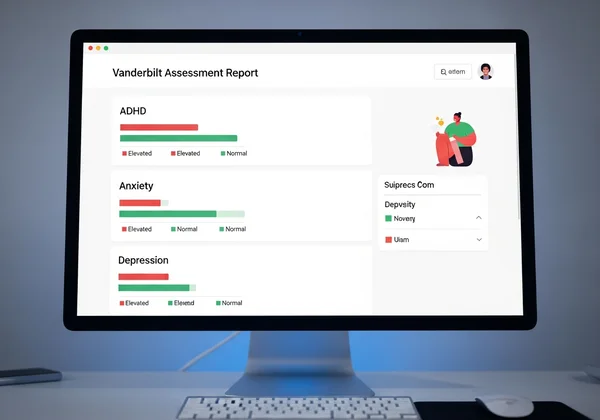
Breaking Down the Inattention Hyperactivity Index vs. Other Condition Scores
The Vanderbilt Assessment report is divided into different sections, or "domains." The primary domain screens for ADHD symptoms (inattention and hyperactivity/impulsivity). The other domains screen for potential co-occurring conditions like ODD, Conduct Disorder, and anxiety/depression.
Each section is scored separately. This means a child can have a high score in the ADHD domain, but low scores in the others. Alternatively, they might have a low score for ADHD but a high score in the anxiety/depression domain. This separation is what makes the tool so useful for getting a nuanced view.
What Elevated Scores in Non-ADHD Domains Might Mean
An elevated score in a non-ADHD domain, such as ODD or anxiety, is a red flag. It indicates that the child is showing a significant number of symptoms related to that condition. This score is calculated based on how many questions in that section were marked as "often" or "very often."
It is important to remember that a high score is a screening result, not a diagnosis. It signals that this is an area of concern that warrants further discussion and evaluation by a qualified professional, like a pediatrician or mental health specialist. Our online tool provides an instant summary, making it easy to see which areas are elevated.
When to Be Concerned About Multiple Elevated Domains
If your child’s report shows high scores in multiple domains—for example, in both ADHD and ODD—it suggests a more complex behavioral picture. This is a strong signal that your child may be dealing with co-occurring conditions.
This information is incredibly valuable. It helps you have a more informed conversation with your child's doctor or school. Instead of just saying "my child has trouble focusing," you can say, "The screening showed concerns in both attention and oppositional behaviors." This allows professionals to move more quickly toward an accurate diagnosis and a comprehensive support plan.
From Assessment to Action: Next Steps for Identified Conditions
Receiving a report with elevated scores can feel overwhelming, but it is also a powerful first step. This information empowers you to seek the right kind of help. Rather than putting labels on your child, the Vanderbilt Assessment helps you better understand their unique needs and create more effective support strategies.
Creating Support Strategies for ODD Behaviors at Home
If the report indicates ODD-related behaviors, there are strategies you can implement at home while seeking professional guidance. These often involve clear, consistent rules and consequences. Using praise for positive behavior and avoiding power struggles can also be very effective. Parent training programs, often recommended by therapists, can provide you with tools to manage these challenging behaviors.
Anxiety Management Techniques for Children with Vanderbilt Indicators
For children showing signs of anxiety, creating a calm and predictable environment is helpful. Simple relaxation techniques, like deep breathing or "belly breathing," can be taught to children to use when they feel worried. Talking openly about their fears without judgment also helps. A therapist specializing in childhood anxiety can teach your child cognitive-behavioral therapy (CBT) techniques to manage their worries.
Addressing Potential Depression Red Flags Through Professional Support
Any sign of depression in a child should be taken seriously. If the Vanderbilt Assessment flags concerns in this area, it is essential to consult a healthcare professional immediately. This is not something to manage on your own. A pediatrician, child psychiatrist, or psychologist can conduct a full evaluation and recommend the best course of action, which may include therapy and other supports.
Your Complete Behavioral Picture with Vanderbilt Assessment
The Vanderbilt Assessment offers more than just ADHD screening—it provides a comprehensive view of your child's behavioral health. It helps identify potential co-occurring conditions that might otherwise go unnoticed. By understanding the full range of indicators assessed—from ODD and anxiety to depression—you can gain valuable insights. This information will guide conversations with healthcare providers and help develop more targeted support strategies for your child.
Taking this screening is your first step toward gaining clarity about your child's behaviors. It turns uncertainty into actionable insights that help you move forward with confidence. Ready to get a complete picture of your child's behavioral health? Take the Vanderbilt Assessment today to understand all aspects of your child's behavior and start on the path to effective support.
Frequently Asked Questions About Vanderbilt Assessment for Co-occurring Conditions
Does the Vanderbilt Assessment diagnose conditions, or is it just a screening tool?
The Vanderbilt Assessment is a highly respected screening tool, not a diagnostic tool. It is designed to identify children who are at risk for ADHD and other behavioral or emotional conditions. A formal diagnosis can only be made by a qualified healthcare professional after a comprehensive evaluation. The results from our online assessment provide a critical starting point for that professional conversation.
How accurate is the Vanderbilt Assessment for identifying non-ADHD conditions like ODD or anxiety?
The Vanderbilt Assessment Scale is widely used and validated for screening ADHD and its common co-occurring conditions. When used correctly, its accuracy is considered good for flagging potential issues with ODD, anxiety, and depression. However, its primary validation is for ADHD, and any elevated scores in other domains should be seen as indicators that require further professional evaluation.
Can a child have high scores in multiple behavioral domains? What does this mean?
Yes, it is common for a child to have high scores in multiple domains. This often indicates the presence of co-occurring conditions. For example, a high score in the ADHD section and the ODD section suggests the child may be struggling with both. This information is vital for healthcare providers, as it points toward a need for a more comprehensive treatment plan that addresses all areas of concern.
How should I discuss potential co-occurring conditions with my child's healthcare provider based on Vanderbilt results?
Bring a copy of the assessment report to your appointment. You can say, "We completed a Vanderbilt Assessment screening, and it showed elevated scores for both inattention and anxiety. I'd like to discuss these results with you and figure out the next steps." This gives the provider specific, structured data to work with, making the appointment more productive.
Are there specific behaviors that indicate a need for immediate professional intervention beyond what the assessment covers?
Yes. While the assessment is a great tool, you should seek immediate professional help if your child talks about self-harm or suicide, shows extreme aggression toward others or animals, or experiences a sudden and dramatic change in personality or behavior. These are serious red flags that require urgent attention from a mental health professional or your local emergency services.